Significant advancements have been made in the therapeutic landscape of cancer, driven by the imperative to develop treatments for patients that are both effective and less toxic. Traditional therapeutic strategies like surgery, chemotherapy, and radiation therapy are generally effective but inherently limited by their lack of specificity regarding the molecular profile of tumors and collateral damage to healthy tissues. These constraints have spurred the pursuit of innovative approaches that leverage the body’s intrinsic defense mechanisms, collectively called immunotherapies. Immunotherapy activates the immune system to recognize and eradicate cancer cells and signifies a paradigm shift in oncology. By enhancing the body’s anti-tumor immune defense, immunotherapy has broadened the therapeutic arsenal and redefined the trajectory of cancer care, offering the potential for durable responses and improved patient outcomes.
The conceptual foundation of immunotherapy dates back over a century, with pioneering observations made by Dr. William Coley in the late 1800s. Coley noted tumor regression in patients with concurrent bacterial infections, suggesting that immune system activation could combat malignancies. Despite the initial promise, his methods, which involved administering bacterial toxins, lacked the mechanistic insights that modern science provides. Advances in immunology throughout the 20th century elucidated key components of the immune response, including T-cells and cytokines, and laid the groundwork for contemporary immunotherapeutic strategies. Checkpoint inhibitors emerged in the early 21st century; these block inhibitory pathways on T-cells that are a safety mechanism to prevent autoimmunity. Ipilimumab (which targets CTLA-4) and nivolumab/pembrolizumab (which target PD-1) showed that blocking immune checkpoints can reinvigorate anti-tumor immunity.
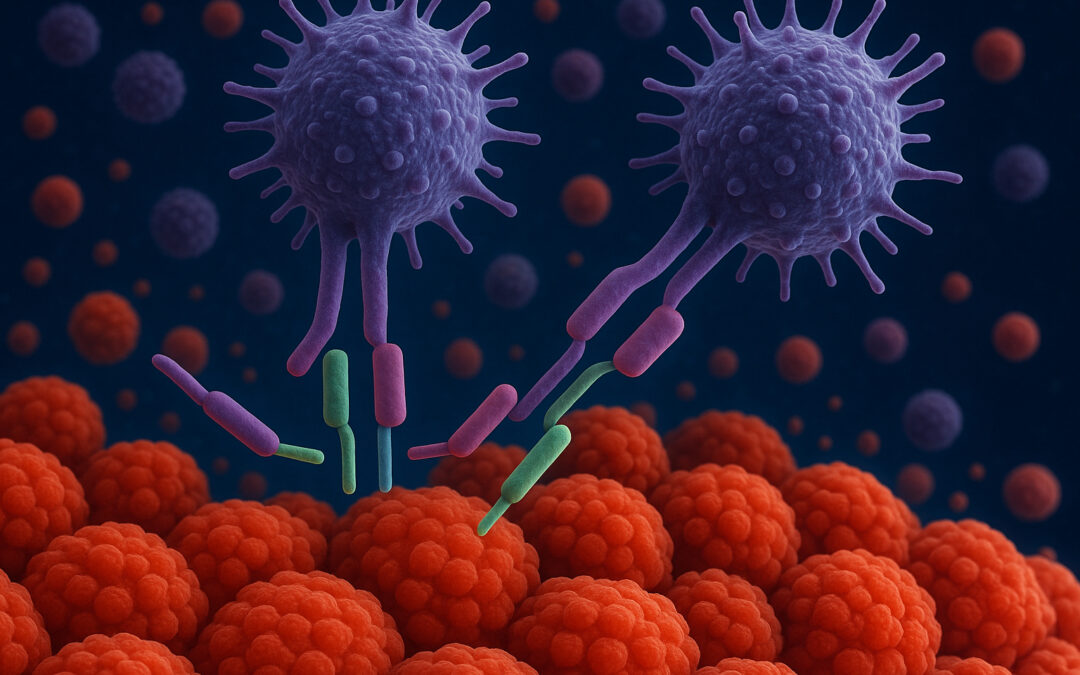
Immunotherapy encompasses several distinct modalities operating through different mechanisms. As mentioned above, checkpoint inhibitors disrupt inhibitory signals that cancer cells exploit to evade immune detection, thereby reinvigorating T-cell activity. Chimeric antigen receptor (CAR) T-cell therapy involves genetically engineering T-cells to express synthetic receptors that recognize tumor-specific antigens, enabling tumor clearance. Monoclonal antibodies bind to surface proteins on cancer cells, tagging them for destruction or blocking proliferative signaling. Cancer vaccines prime the immune system to recognize tumor-specific antigens, while cytokine therapies such as interleukin-2 and interferons amplify immune responses, enhancing tumor eradication.
Non-small cell lung cancer (NSCLC), the most common subtype of lung cancer, has experienced significant advancements due to immunotherapy. Drugs like pembrolizumab and nivolumab have become the standard of care, particularly for tumors with high PD-L1 expression. These therapies promote T-cell activation by disrupting the PD-1/PD-L1 axis, fostering more robust and sustained anti-tumor immune responses. Clinical trials have demonstrated that immunotherapy often surpasses chemotherapy in both efficacy and tolerability, representing a paradigm shift in the management of NSCLC.
Although immunotherapy has achieved notable successes, its effectiveness is inconsistent across all cases, making real-time monitoring of therapeutic responses essential for optimizing clinical outcomes. Traditional imaging techniques may fall short in promptly and accurately portraying therapeutic responses, especially in patients with heterogeneous responses or stable disease. Liquid biopsies have emerged as a minimally invasive alternative, analyzing circulating tumor DNA (ctDNA) molecules shed by tumor cells into the bloodstream. Longitudinal tracking of fluctuations in ctDNA levels enables clinicians to assess systemic tumor burden and treatment efficacy precisely. These approaches can elucidate the heterogeneity of immunotherapy responses and facilitate timely therapy modifications. Concurrently, monitoring T-cell activation and differentiation patterns provides insights into the immune system’s engagement, revealing proliferation, exhaustion, and memory formation markers correlating with differential therapeutic outcomes or the emergence of immune-related toxicities.
In conclusion, immunotherapy has redefined the field of oncology, harnessing the immune system to achieve targeted and durable anti-tumor responses. Its success is exemplified by breakthroughs in NSCLC treatment, where checkpoint inhibitors have improved clinical outcomes compared to traditional chemotherapy for many patients. However, timely and accurate capture of therapeutic response remains a challenge. Liquid biopsies and immune cell population profiling represent pivotal advancements in combating this challenge. Ongoing research is honing these technologies, enabling synergies between immunotherapy and real-time molecular monitoring of treatment response, ultimately leading to improved outcomes with precision immuno-oncology.
References:
- Pardoll, D.M. (2012). The blockade of immune checkpoints in cancer immunotherapy. Nature Reviews Cancer, 12(4), 252-264.
- Topalian, S.L., et al. (2012). Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. New England Journal of Medicine, 366(26), 2443-2454.
- Ribas, A., & Wolchok, J.D. (2018). Cancer immunotherapy using checkpoint blockade. Science, 359(6382), 1350-1355.
- June, C.H., O’Connor, R.S., Kawalekar, O.U., Ghassemi, S., & Milone, M.C. (2018). CAR T cell immunotherapy for human cancer. Science, 359(6382), 1361-1365.
- Aredo J.V. et al. Liquid Biopsy Approaches for Cancer Characterization, Residual Disease Detection, and Therapy Monitoring. Am Soc Clin Oncol Educ Book 45, e481114 (2025). DOI:10.1200/EDBK-25-481114
- Anagnostou, V., Ho, C., Nicholas, G. et al. ctDNA response after pembrolizumab in non-small cell lung cancer: phase 2 adaptive trial results. Nat Med 29, 2559–2569 (2023). https://doi.org/10.1038/s41591-023-02598-9